Is Microdiscectomy a Major Surgery?
Share this Post to earn Money ( Upto ₹100 per 1000 Views )
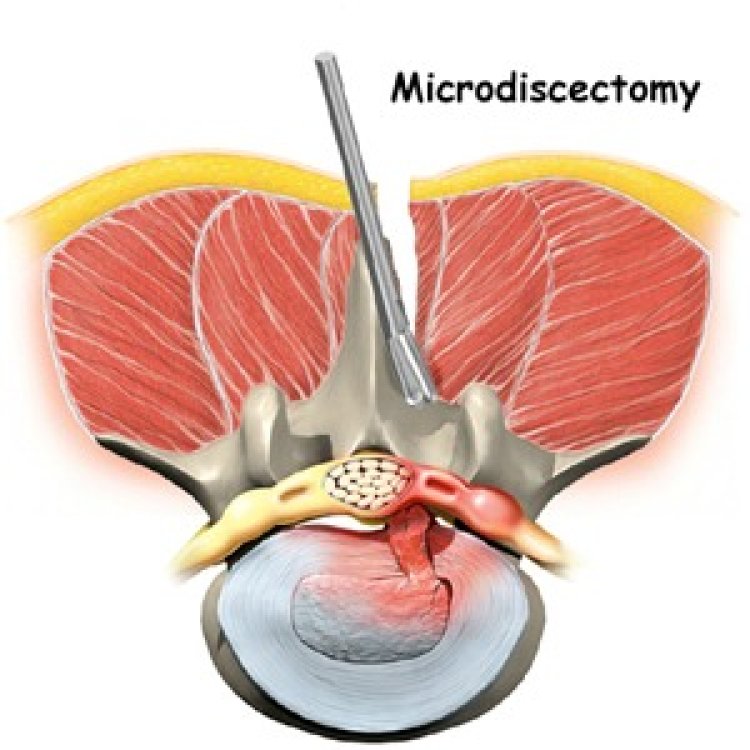
Microdiscectomy is a minimally invasive surgical procedure used to relieve pressure on a spinal nerve root caused by a herniated disc in the lower spine. It is one of the most common surgeries for treating sciatica or nerve compression resulting from disc herniation. The term "microdiscectomy" refers to the use of a microscope or magnification to help guide the surgeon in removing the damaged portion of the disc while minimizing trauma to surrounding tissues. Hospitals such as Sir HN Reliance Hospital Mumbai offer this advanced procedure as part of their specialized spinal care services. While it is often labeled as "minimally invasive," there is still a debate about whether microdiscectomy qualifies as major surgery.
In this article, we will explore the procedure, its risks, recovery, and why it may or may not be considered major surgery.
What is Microdiscectomy?
Microdiscectomy involves the surgical removal of the portion of a herniated disc that is compressing a nerve in the spinal column. When a disc herniates, the inner gel-like material of the disc pushes through its outer wall, pressing against the spinal nerves. This leads to pain, numbness, weakness, and sometimes loss of function, particularly in the legs (sciatica).
In a microdiscectomy, the surgeon makes a small incision, usually around 1 to 1.5 inches long, in the lower back. Using a microscope or magnification, the surgeon carefully moves muscles and tissues aside to expose the affected nerve and disc. Only the portion of the disc causing nerve compression is removed, leaving the rest of the disc intact.
Is Microdiscectomy Considered Major Surgery?
To answer whether microdiscectomy is major surgery, it’s essential to define what "major surgery" entails. In general, major surgeries involve:
- General anesthesia.
- Invasive procedures that enter the body’s cavities.
- Risk of significant blood loss.
- A long recovery period.
- Potential for serious complications.
Microdiscectomy does meet some of these criteria, but it falls into a gray area between minor and major surgery due to its minimally invasive nature. Here’s a breakdown of the factors that make it a borderline case:
-
General Anesthesia
Microdiscectomy is typically performed under general anesthesia, which is a hallmark of major surgeries. General anesthesia carries inherent risks, including reactions to medications, breathing problems, and in rare cases, more severe complications. The need for anesthesia is one of the reasons some medical professionals classify microdiscectomy as major surgery. -
Invasiveness
While microdiscectomy is less invasive than traditional open spine surgery, it still requires an incision and the manipulation of tissues to access the spine. However, the use of advanced techniques and smaller incisions reduces the overall trauma to the body. This is why some experts consider it a minimally invasive procedure rather than a full-scale major surgery. -
Blood Loss
One of the significant differences between microdiscectomy and more invasive spinal surgeries is the amount of blood loss. With microdiscectomy, the blood loss is minimal, which is a reason it might not be classified as a major surgery. Less tissue is disrupted, and the smaller incision size means quicker healing and less bleeding overall. -
Recovery Time
Recovery from microdiscectomy is generally quicker than from traditional open surgeries. Patients are often able to return home the same day or after a short hospital stay, and full recovery can take anywhere from two to six weeks, depending on the individual and their activity level. In comparison, more invasive surgeries like spinal fusions require longer recovery times and extended hospital stays. The relatively short recovery period of microdiscectomy further supports its classification as a minimally invasive surgery. -
Risk of Complications
Like any surgery, microdiscectomy carries risks. These include infection, bleeding, nerve damage, or recurrence of the herniation. However, these risks are lower than in more invasive spinal procedures. Still, because the surgery involves the spine and nerves, the potential for complications can be serious, which leans toward classifying it as major surgery in some cases.
Benefits of Microdiscectomy
The minimally invasive nature of microdiscectomy offers several advantages over more traditional spinal surgeries:
- Smaller Incisions: This results in less scarring and a quicker recovery.
- Reduced Muscle Damage: The muscles surrounding the spine are gently moved aside rather than cut, preserving their function and strength.
- Shorter Recovery Time: Most patients can return to normal activities, including work, within a few weeks of the surgery.
- Lower Risk of Infection: With a smaller incision and less disruption of tissues, the risk of infection is reduced.
Is Microdiscectomy Right for You?
Microdiscectomy is typically recommended for individuals who have not found relief from non-surgical treatments such as physical therapy, medications, or injections. The procedure is especially useful for patients with leg pain (sciatica) caused by a herniated disc that has not improved after 6-12 weeks of conservative treatment. However, it is important to consult with a spine specialist to assess the risks and benefits in your specific case.
Conclusion
While microdiscectomy is often described as a minimally invasive surgery, it does share some characteristics of major surgery, such as the use of general anesthesia and the involvement of critical structures like nerves and the spine. However, its smaller incision size, reduced tissue trauma, and quicker recovery time make it less invasive than traditional spinal surgeries. Ultimately, whether microdiscectomy is classified as major surgery may depend on the context, but in many ways, it strikes a balance between the two, offering a safe and effective option for relieving pain from herniated discs.